Like us on Follow Us on
Follow Us on  Caregiver Blog
Caregiver Blog![]()
DISCLAIMER ...
There is no hard and fast answer to addressing a problem behaviour.
The following information is provided as a tool to help the Caregiver find the solution that works for situation they are faced with.
Problem Behaviours - Introduction
Between 80% – 90% of those with Alzheimer’s will develop some behavioral symptoms.
Alzheimer’s disease causes brain cells to die, so the brain works less well over time. This changes how a person acts. There are a number of recognised behaviour problems associated with Alzheimer's disease. These problems can interfere with normal daily activity and sleep and may increase the risk of harm to the person with Alzheimer's and their caregiver.
This section is provided as a resource to Caregiver's looking for possible causes and coping strategies to help deal with the day-to-day struggle. Each of the behaviour pages is divided into three specific areas. It is hoped that caregivers may find some help in dealing with their own situation:
Anger
Hallucinations / Paranoia
Incontinence
Bathing
Dressing
Eating
Sleeping
Repetitive Actions
Verbal / Screaming
Wandering
Wanting to 'Go Home'
General Overview
As a caregiver for a loved one with dementia, it can be extremely worrying and upsetting to experience the behavior problems associated with mid-stage Alzheimer’s disease. Patients may exhibit a wide variety of behavioral problems that can threaten their own or other people’s safety, including wandering, aggressiveness, hallucinations, or sleeping and eating problems.
While it’s not always easy to understand unexpected outbursts or erratic and aggressive actions, many behavior problems are made worse by a poor environment and an inability to deal with stress. By learning how to make changes in the home environment and caring atmosphere, you can help to reduce stress, improve problem behavior, and increase the quality of life for both the patient and yourself.
Awareness and management of difficult behaviors by the Caregiver becomes an important means of dealing with stress and easing tension between the care receiver and the caregiver. For the sufferer these behaviors are an effort to communicate that something is wrong, not an effort to be difficult. Dementia is a progressive, increasingly debilitating illness. Therefore, the treatment must adjust to the individual, rather than be seen as a concrete set of rules that will remain unchanged over time.
Each individual is impacted differently, with the loss of function in no straight line. In other words, any attempt to devise one program of standardized care for Dementia would be the same as deciding that everyone diagnosed with cancer should have exactly the same treatment.
Problem behavior is often a way the Alzheimer’s patient tries to communicate with you. The progression of the disease means that they may no longer be able to communicate verbally, but they are still emotionally conscious and will remain so, often until the very end of life.
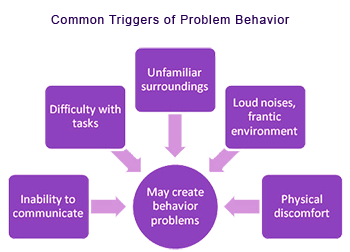
In many cases the patient’s behavior is a reaction to an uncomfortable or stressful environment. If you can establish why the patient is stressed or what is triggering their discomfort, you should be able to resolve the problem behavior with greater ease. Remember that the person with dementia is not being deliberately difficult. Their sense of reality may be different to yours, but it’s still very real to them.
Some ways to help identify the causes of problem behavior:
Problem behaviors have as their basis two sets of factors:
Internal factors: |
External factors: |
|---|---|
|
|
OUR STORY
A Family Reflection And A Promise Kept
THE CAREGIVER ROLE
What is a Caregiver
The Caregiver Defined
Who Do Caregivers Care For
Accepting the Reality of Dementia
6 Steps to Successful Caregiving
Caregiver's Are Not Alone
Asking For & Getting Help
The Caregiver Code
Rights of a Caregiver
General Suggestions
Unmet Needs Of A Caregiver
Caregiver And Work
Feelings And Caregiver Stress
Questions & Answers
Notable People
STRESS, COPING & FEELINGS
The Caregiver Code
Rights of The Caregiver
Coping With Stress
Feelings And Caregiver Stress
Stages Of Alzheimer's
Helping Children Understand
Caregiver Burnout
Protecting Yourself From Burnout
Making Time For Reflection
Moving On
How is Competency Defined?
Power of Attorney
What is an Advanced Directive?
Do I Really Need a Will or a Trust?
COMMUNICATION
Importance of Communication
Communicating With Someone Who Has Alzheimer's
Your Approach Sets The Tone
Think Before You Speak
Doing Tasks Together
Having Trouble Being Understood
Keeping a Dementia Journal
Making Caregiving Easier - Caregiver Notebook
Things NOT To Do
When It Just Fails
ALZHEIMER'S BASICS
What is Alzheimer's
Why is Alzheimer's Different
Stages of Alzheimers
Can Alzheimers be Inherited
Statistics
The Mortality Question
TIPS AND ISSUES
New To Family Caregiving?
Tips For Dealing with Aggression
Places To Turn For Caregiver Supoort
Take Advantage of Community Support
Random Tips From Other Caregivers
Providing Long Distance Care
When To Stop Driving
Dealing With Family
Conflict
Tips on Sundowning
Ways to Reduce Sundowning Challenges (part A)
Ways to Reduce Sundowning Challenges (part B)
Helping Children Understand
Pet & Toy Therapy
Fixations
Getting Someone to Take Medications
Tips For Medical Appointments
Dealing With Resistance
Tips For Day To Day
Intimacy And Sexuality
Visiting A Person With Dementia
Music And Dementia
Tips For Holidays And Gatherings
Art as Home Therapy
PROBLEM SOLVING
What Can I Do To Be A More Effective Caregiver
Planning Tips
Dealing with False Dementia Accusations
Responding to Common Dementia Accusations
Steps to Effective Problem Solving
PROBLEM BEHAVIOURS
Anger
Hallucinations / Paranoia
Incontinence
Bathing
Dressing
Eating
Sleeping
Repetitive Actions
Verbal / Screaming
Wandering
Wanting to 'Go Home'
RESEARCH & DONATIONS